ITI Milestones
The Very Beginning
“Two things made ITI possible. One was research that The Edna McConnell Clark Foundation supported, which verified that the four elements of the SAFE strategy were individually effective, and which packaged them all together...The second thing was the availability of Zithromax, and the willingness of Pfizer to take a chance on giving this drug away. What we needed was a single-dose effective antibiotic."
- Dr. Joseph Cook, Tropical Disease Research Program Director,
Edna McConnell Clark Foundation (1978-1999),
former ITI Director (1998-2003)
We Need a Plan
"Our scientists came back extremely excited about this development and keen to do something. It seemed to us that there was a real contribution we could make. We didn't know how big it would be. We didn't know how many people had trachoma. We didn't know how widespread it was, though we knew it was widespread and mainly in developing countries. So we said, 'Okay, we'll do something.'"
- C.L. Clemente, Executive Vice President, Corporate Affairs, Pfizer (1992-2002),
ITI Board Chair, (1998-2004)
Breakthrough Treatment
"An important milestone was the Global Scientific Meeting on Trachoma Control in 1996 that was convened by WHO, with very strong support from The Edna McConnell Clark Foundation. This was the time when it was very clear that azithromycin would present a major breakthrough in terms of antibiotic treatment for trachoma. A defining consensus at the end of the meeting was to say that we should set up a kind of mechanism, a structure that would allow having the different stakeholders around a table in order to discuss trachoma control."
- Dr. Serge Resnikoff, Former Coordinator,
Chronic Disease Prevention and Management,
WHO Member,
former ITI Trachoma Expert Committee
Introducing the International Trachoma Initiative
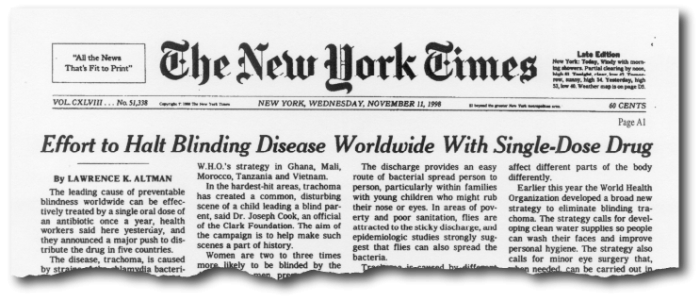
The amplifying mechanism for the global programme was the WHO Alliance for the Global Elimination of Trachoma by 2020 (GET2020), a large partnership of WHO Member States, non-governmental organizations, research institutions, philanthropic foundations, and industry. In 1998, the 2020 target was set by the World Health Assembly (WHA), which passed resolution WHA 51.11, signed by all 193 Member States to commit to ending blinding trachoma.
On November 10, 1998, Pfizer and The Edna McConnell Clark Foundation announced the formation of the International Trachoma Initiative as the world's only nonprofit organization solely devoted to eliminating blinding trachoma.
Antibiotic Distribution Begins
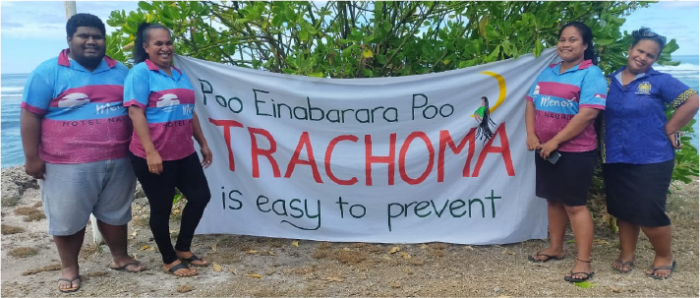
Tanzania and Morocco were the first countries to receive donated antibiotics. In Tanzania, the acronym SAFE has been translated to SAFI, the Kiswahili word for "good," "clean," or "nice." The Kiswahili slogan for the Tanzania trachoma campaign was "Uso SAFI? Poa!!"or "Clean face? Cool!!"
"We integrated trachoma into the work of every government agency. We created a model lesson for the schools. We made films to encourage people to think about the cleanliness of their wells, and we asked the National Office of Potable Water (ONEP) to show our films. We gave posters to our health care workers and offered to provide communications training to workers in any agency. We taught them how to communicate about their projects and educated them about trachoma control and prevention."
- Dr. Youssef Chami-Khazraji,
Director of the Division of Communicable Diseases,
Department of Epidemiology & Disease Control,
Ministry of Health, Morocco.
Quick Facts for 1999
- New countries: Tanzania and Morocco
- Cumulative shipments: 1,107,984
- Number of countries served: 2

Quick Facts for 2000
- New countries: Mali, Sudan, and Vietnam
- Cumulative shipments: 2,478,211
- Number of countries served: 5

Quick Facts for 2001
- New countries: Egypt, Ghana, Nepal, and South Sudan
- Cumulative shipments: 4,794,474
- Number of countries served: 9

Quick Facts for 2002
- New countries: Ethiopia and Niger
- Cumulative shipments: 8,668,086
- Number of countries served: 11

Pfizer Expands Donations
In 2003, Pfizer increased drug donation from 10 million doses in ITI's first five years to 35 million for the next five, greatly facilitating ITI's expanded support for the global programme.
Quick Facts for 2003
- New countries: Mauritania
- Cumulative shipments: 15,544,733
- Number of countries served: 12

International Coalition for Trachoma Control (ICTC) is Established
"We can do so much more when we do it together."
-Catherine Cross, First Chair of ICTC
The beauty of the ICTC lies in the inclusive and collaborative operating model that plays to the strengths of partners, allowing them to focus their efforts on supporting countries instead of competing for funds. The collaborative approach gives us a comparative advantage in every aspect of our work - whether it be data collection, resource mobilization, and sharing best practices. New and expanding country programs could avoid the pitfalls of pilot phases, learn from the experiences of neighboring countries, and go straight to scale-up.
Quick Facts for 2004
- New countries: Senegal
- Cumulative shipments: 36,294,044
- Number of countries served: 13

Celebrity Endorsement
Model Cheryl Tiegs joined forces with ITI by serving as an advocate for trachoma elimination. Her visit to Ghana resulted in local and international press coverage, and galvanized government support for the elimination of trachoma.
Quick Facts for 2005
- Cumulative shipments: 51,285,143
- Number of countries served: 13

USAID Support
Through USAID, the U.S. government took their first steps towards becoming the single greatest supporter of MDAs for trachoma elimination. The number of antibiotics donated rose from 81 million total doses between 1999 and 2005 to almost a billion total doses between 2006 and 2021.
Quick Facts for 2006
- New countries: Kenya and The Gambia
- Cumulative shipments: 80,826,887
- Number of countries served: 15

100 Million Doses Milestone Reached
In 2007, the cumulative number of doses of the Pfizer donated antibiotics shipped by ITI exceeded 100 million doses.
Quick Facts for 2007
- New countries: Burkina Faso and Uganda
- Cumulative shipments: 114,212,057
- Number of countries served: 17
ITI Celebrates 10 Year Anniversary
"Among ITI's major accomplishments from 2003 to 2007 was a strategic shift in ITI's role in trachoma elimination. We moved from ITI-owned programs to government-owned, government-led and government-supported programs. We began to implement SAFE support in 12 countries. This meant scaling up mass drug administration from 1.5 million people in 2002 to more than 25 million four years later. Most importantly, we saw community empowerment. The lives of people in several communities where SAFE was implemented had been transformed. In addition to a drastic reduction in the prevalence of trachoma, we saw less respiratory disease and diarrhea in children, greater use of latrines, cleaner faces, and fewer flies."
- Dr. Jacob Kumaresan, former ITI President (2003-2007)
Quick Facts for 2008
- New countries: Guinea Bissau
- Cumulative shipments: 149,847,285
- Number of countries served: 18

ITI Joins The Task Force for Global Health
"The mission and goals of ITI are a strong complement to the Task Force mission. We are at an important juncture for trachoma control efforts and this commitment from Pfizer to supply antibiotics will help mobilize the partners essential to the success of this mission.”
- Dr. Mark Rosenberg, former President & CEO of The Task Force for Global Health (2000-2016)
Quick Facts for 2009
- New countries: Eritrea
- Cumulative shipments: 189,870,933
- Number of countries served: 19

Looking Forward
"We only have ten years left to reach the goal of eliminating blinding trachoma. In order to achieve this, all endemic countries must have the full scale SAFE strategy in place by 2015 to allow enough time for implementation to have an impact. Enormous challenges lie ahead of us. Some of the remaining endemic countries are in conflict or have just come out of conflict, and lack infrastructure and resources to fully address the disease. Even countries free of conflict lack financial resources for the epidemiological surveys to determine which districts need intervention, or to support intervention in endemic districts...However, we believe that, together, we can overcome these challenges and reach our goal."
- Dr. Danny Haddad, former ITI Director (2009-2013)
Quick Facts for 2010
- New countries: Burundi, Nigeria, Zambia
- Cumulative shipments: 244,058,917
- Number of countries served: 22
ITI Publishes The End in Sight: 2020 INSight
This collaborative road map between national programs and implementing partners infused new energy into trachoma elimination efforts.
“After INSight 2020, we realized we needed quality assurance, standardization, and huge scale up. That was when we decided to use some strategic reserve funds to kick-start the global mapping and standardization process.”
- Dr. Danny Haddad, former ITI Director (2009-2013)
“To eliminate any disease, the critical step is knowing where the disease is - otherwise you’re just shooting in the dark.”
- Dr. Anthony Solomon, Lecturer, London School of Hygiene & Tropical Medicine (1999-2014)Medical Officer, Neglected Tropical Diseases, WHO
Quick Facts for 2011
- New countries: Cameroon and Malawi
- Cumulative shipments: 293,200,933
- Number of countries served: 24

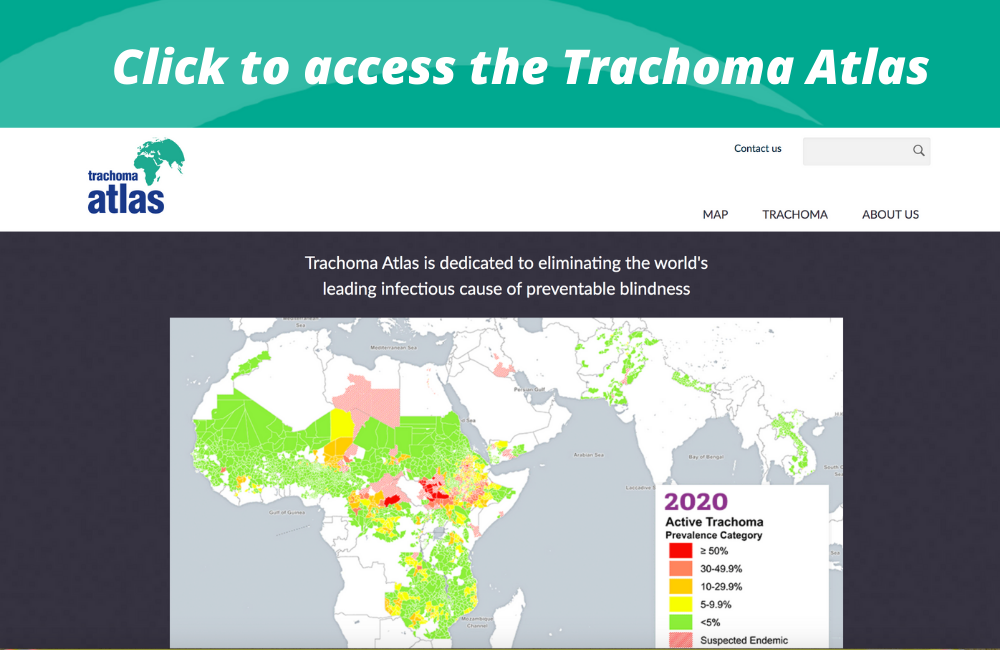
Global Trachoma Mapping Project is Launched
ITI and a consortium of partners supported the development of the Global Trachoma Mapping Project (GTMP), a standardized methodology conforming to WHO guidelines for data collection based on a mobile platform to gather disease prevalence data and allowing analysis on a real-time basis.
These data have been made available on the ITI-managed Trachoma Atlas at www.trachomaatlas.org.
Consistent with the large scale-up, the Zithromax supply chain was streamlined by shipping 500 count bottles. The large bottles replaced the previous 30-tablet ones reducing transport costs and the required storage space. Each full pallet of bottles of tablets increased from 33,600 doses to 215,000.
Quick Facts for 2012
- New countries: Central African Republic, Chad, Guinea, Mozambique, and Solomon Islands
- Cumulative shipments: 346,522,629
- Number of countries served: 29

"With the help of Pfizer, we are trying to eliminate blinding trachoma from the face of the Earth by 2020. I think we have a very good chance of reaching this goal."
- The Honorable Jimmy Carter, 39th President of the United States and Founder of The Carter Center
15th Anniversary Celebration
ITI celebrated its 15th year with Carter Center colleagues at the Pfizer Headquarters in New York to mark a shared vision for trachoma elimination.
"We are gratified about the progress that has been made toward eliminating trachoma as a public health concern."
- Ian Read, Former Chairman and CEO, Pfizer
Quick Facts for 2013
- New countries: Guatemala
- Cumulative shipments: 398,353,877
- Number of countries served: 30

Ethiopia Hosts GET 2020 Meeting
The 18th annual meeting of GET 2020 was hosted by the Government of Ethiopia in Addis Ababa. This raised the profile of the trachoma program and galvanized domestic funding and support.
"We have a tremendous opportunity to leave the world a better place than we found it, and with that opportunity, a great responsibility to ensure the resources entrusted to us get to the people who need them."
- Dr. Paul Emerson, ITI Director
Quick Facts for 2014
- Cumulative shipments: 444,740,167
- Number of countries served: 30

Half a Billion Doses Milestone Reached
In November 2015, the 500 millionth dose of donated antibiotics was shipped to trachoma-endemic countries, smashing the 1998 target of 10 million!
The Global Trachoma Mapping Project reached a milestone of over 1 million people screened for clinical signs of trachoma in 29 countries.
ITI and Ministries of Health from Ethiopia, Eritrea, Kenya, South Sudan, Sudan, Tanzania, and Uganda met in Kenya for the first annual NTD and trachoma cross-border meeting. Since then, similar groups have been formed for Southern Africa and Francophone countries.
Quick Facts for 2015
- Cumulative shipments: 507,124,255
- Number of countries served: 30

Outreach Expansion
2016 was the first year in which over 100 million doses of antibiotics were shipped to endemic countries. The number of doses shipped in 2016 alone exceeded the cumulative total shipped in the first ten years of ITI.
Over 85 million people received treatment in 2016.
ITI with partners RTI International and Sightsavers supported the launch of Tropical Data, a consortium of scientific, technological and implementation partners to work alongside Ministries of Health to support rigorous epidemiological surveys to conform to WHO guidelines for data collection.
Quick Facts for 2016
- New countries: Benin, Cote d'Ivoire, Democratic Republic of the Congo, Kiribati, Vanuatu, and Zimbabwe
- Cumulative shipments: 627,860,465
- Number of countries served: 36

Zithromax® Shipment Tracker Launched
Over 700 million doses of antibiotics have been donated to trachoma endemic countries since 1999.
ITI launched The Zithromax® Shipment Tracker which gave on-demand access to information about recent and upcoming shipments; the quantities of drugs requested via the annual drug requests; current decisions made by the Trachoma Expert Committee; quantities shipped year-to-date; quantities remaining to be shipped; expected arrival date; and mode of transport.
Over 1 million people were screened for clinical signs of trachoma using the Tropical Data service for trachoma prevalence surveys.
Quick Facts for 2017
- New countries: Colombia, Fiji, and Pakistan
- Cumulative shipments: 709,241,739
- Number of countries served: 39

20th Anniversary Celebration
ITI celebrated 20 years of working for a world free from trachoma and the exciting news that there has been a 50% reduction in the global burden of trachoma. More good news, Pfizer extends Zithromax® donation to 2025 to reach most marginalized communities.
Watch the 20th Anniversary documentary
Quick Facts for 2018
- New countries: Yemen
- Cumulative shipments: 810,777,123
- Number of countries served: 40
Zithromax® Guidelines Published
ITI Published the Zithromax® Management Guide with the goal of enhancing safety, ease, and acceptability of Zithromax® administration. The Guide is designed for all stakeholders at all levels who use donated Zithromax® for trachoma elimination. Access the Zithromax® Management Guide.
Quick Facts for 2019
- Cumulative shipments: 897,718,347
- Number of countries served: 40
Trachoma Elimination During the Pandemic
In the midst of the COVID-19 pandemic, one of the many highlights of 2020 involved ITI delivering the country of Nauru its first-ever Zithromax® shipment; from Brussels to Singapore to Brisbane to Nauru, the shipment included 14,448 treatments with a total distance of 12,451 miles. Nauru conducted its first trachoma mass drug administration (MDA) in May 2020 and wrapped up MDAs in June 2020. Read the full story.
Quick Facts for 2020
- New countries: Nauru
- Cumulative shipments: 928,868,255
- Number of countries served: 41
ITI Performance Metrics in 2023

Zithromax® Shipments
1999–Present
As of March 8, 2024
As of March 8, 2024
Progress in Our Global Program
MASS DRUG ADMINISTRATIONS (MDAS): We maximize the potential for elimination by treating many people at once.
SCALING DOWN: We are succeeding in reducing the need for Zithromax® distribution through SAFE measures.

People no longer requiring Zithromax® for trachoma as of May 2023
GLOBAL IMPACT: We are reducing the global burden of trachoma one country at a time.

Countries validated for trachoma elimination as of July 2023